Methotrexate
Methotrexate decreases the activity of the immune system and slows cancer cell growth. Reserved for conditions that cannot be treated with other medications.
Methotrexate Overview
Methotrexate is a prescription medication used to treat certain types of cancers. It is also used to treat psoriasis, polyarticular juvenile idiopathic arthritis (PJIA), and rheumatoid arthritis (RA).
Methotrexate belongs to a group of drugs called antimetabolites. It decreases the activity of the immune system and slows the growth of cancer cells. Methotrexate treats psoriasis by slowing the growth of skin cells to stop scales from forming. Methotrexate may treat rheumatoid arthritis by decreasing the activity of the immune system.
This medication comes in tablet form and can be taken with or without food. It also comes in an oral solution form that can be taken with or without food.
This medication is also available as a powder to be mixed with liquid to be injected intramuscularly (into a muscle), intravenously (into a vein), intra-arterially (into an artery), or intrathecally (into the fluid-filled space of the spinal canal).
Common side effects of methotrexate include nausea, dizziness, drowsiness, and headache. Do not drive or operate heavy machinery until you know how this medication affects you.
How was your experience with Methotrexate?
Methotrexate Cautionary Labels
Uses of Methotrexate
Oral/Injectable:
Methotrexate is a prescription medication used to treat the following conditions:
- severe psoriasis
- rheumatoid arthritis
- polyarticular juvenile idiopathic arthritis (PJIA)
- breast cancer
- certain types of head and neck cancer
- acute lymphoblastic leukemia (ALL)
- advanced non-Hodgkin lymphoma (NHL)
- advanced mycosis fungoides (a type of cutaneous T-cell lymphoma)
- osteosarcoma that has not spread to other parts of the body, following surgery to remove the primary tumor
Methotrexate is also used to treat the following types of gestational trophoblastic tumors:
- Chorioadenoma destruens
- Choriocarcinoma
- Hydatidiform mole
This medication may be prescribed for other uses. Ask your doctor or pharmacist for more information.
Methotrexate Brand Names
Methotrexate Drug Class
Methotrexate is part of the drug class:
Side Effects of Methotrexate
Oral/Injectable:
See "Methotrexate FDA Warning" for the most serious reactions.
Methotrexate may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- dizziness
- drowsiness
- headache
- swollen, tender gums
- decreased appetite
- reddened eyes
- hair loss
- fever
- chills
- increased risk of infection
Some side effects can be serious. If you experience any of these symptoms, call your doctor immediately:
- vomiting
- blurred vision or sudden loss of vision
- sudden fever, severe headache, and stiff neck
- seizures
- confusion or memory loss
- weakness or difficulty moving one or both sides of the body
- difficulty walking or unsteady walking
- loss of consciousness
- impaired speech
- decreased urination
- swelling of the face, arms, hands, feet, ankles, or lower legs
- hives
- itching
- skin rash
- difficulty breathing or swallowing
This is not a complete list of this medication’s side effects. Ask your doctor or pharmacist for more information.
Tell your doctor if you have any side effect that bothers you or that does not go away.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Methotrexate Interactions
Tell your doctor about all the medicines you take including prescription and non-prescription medicines, vitamins and herbal supplements. Especially tell your doctor if you take:
- nonsteroidal anti-inflammatory drugs (NSAIDS) such as aspirin, choline magnesium trisalicylate (Tricosal, Trilisate), ibuprofen (Advil, Motrin), magnesium salicylate (Doan's), naproxen (Aleve, Naprosyn) or salsalate.
- acitretin (Soriatane)
- azathioprine (Imuran)
- isotretinoin (Accutane)
- sulfasalazine (Azulfidine)
- tretinoin (Vesanoid)
- chloramphenicol
- oral Antibiotics such as amoxicillin (Moxatag), ampicillin (Omnipen), trimethoprim/sulfamethoxazole (Bactrim, Septra), cephalexin (Keflex), azithromycin (Zithromax), clindamycin, doxycycline (Vibramycin), ciprofloxacin (Cipro), levofloxacin (Levaquin)
- penicillin
- tetracycline
- folic acid
- phenytoin (Dilantin)
- probenecid (Benemid)
- sulfadiazine
- sulfamethizole (Urobiotic)
- sulfisoxazole (Gantrisin)
- and theophylline (Theocron, Theolair)
This is not a complete list of methotrexate drug interactions. Ask your doctor or pharmacist for more information.
Methotrexate Precautions
Serious side effects have been reported with Xatmep including the following:
- Low blood cell counts. This medication can affect your bone marrow and cause you to have low blood cell counts. Your doctor will do blood tests as needed to check your blood cell counts
- Serious infection. This medication can increase your risk of developing life-threatening bacterial or viral infection from opportunistic bacteria. Tell your healthcare provider if you have any of the following symptoms
- fever
- fatigue
- nausea/vomiting
- rash
- Decline in kidney function. Toxicity from Xatmep may occur with kidney dysfunction. Your doctor may want to monitor your kidneys with certain blood tests. Tell your healthcare provider right away if you have any of the following symptoms of kidney dysfunction:
- swelling of face, ankles, hand, or feet
- fatigue
- pale skin
- decreased urination
- shortness of breath
- change in blood
- Stomatitis. Notify your healthcare provider right away if you have any of the following symptoms:
- redness
- swelling
- sores in the mouth
- Decline in liver function. Tell your doctor about any signs or symptoms of liver damage including the following:
- loss of appetite or weight loss
- nausea/vomiting
- feeling tired
- stomach pain/tenderness
- dark urine
- yellowing of the skin or the whites of your eyes
- fever or rash
- Lung Toxicity. Call your healthcare provider if you experience any of the following symptoms:
- shortness of breath
- coughing up mucus
- chest tightness
- pain with breathing
- Severe Allergic Reactions. Tell your healthcare provider about any signs or symptoms of severe allergic reaction:
- chest pain
- swelling of the face, eyes, lips, tongue, arms, or legs
- difficulty breathing or swallowing
- rash
- Secondary Cancers. An increased risk of developing other cancers.
- Harm to Your Unborn Baby. Xatmep can cause harm and potential death to your baby. Consider the risk and benefit of using Xatmep in pregnant women.
- Live Vaccines. Using live vaccines while on Xatmep is not recommended. Talk to your doctor about which vaccines work best for you.
- Impaired Fertility. Xatmep can cause menstrual dysfunction and affect successful pregnancy.
- Accumulation. Xatmep can accumulate in the space between cells and change how other medications work. You could have increased chance of toxicity or side effects.
- Bone Toxicity. If Xatmep is used at the same time as radiation therapy, there is an increased risk of bone infection.
- Laboratory Tests. Xatmep therapy requires significant laboratory testing including blood, lung, and liver testing frequently.
- Improper Dosing. The dosing for Xatmep is weekly, not daily. Daily dosing is associated with an increased risk of death or severe side effects.
Oral/Injectable:
- Do not drink alcohol while taking methotrexate. Alcohol can increase your risk of liver problems.
- Talk to your doctor before receiving immunizations (vaccinations).
- Do not take NSAIDS (nonsteroidal anti-inflammatory drugs) such as aspirin, ibuprofen, or naproxen without first checking with your doctor.
- Methotrexate may lower the number of white blood cells in your blood, increasing your risk for getting an infection. Avoid people with known infections. Avoid touching your eyes or nose. Wash your hands often.
- Methotrexate may increase your risk of bleeding by lowering the number of platelets in your blood. Tell your doctor right away if you notice any unusual bleeding or bruising.
- Methotrexate may make your skin sensitive to sunlight or ultraviolet light. If you have psoriasis, your sores may get worse if you expose your skin to sunlight while you are taking methotrexate. Plan to avoid unnecessary or prolonged exposure to sunlight or ultraviolet light (tanning beds and sunlamps) and to wear protective clothing, sunglasses, and sunscreen.
- Methotrexate may cause dizziness or make you feel drowsy. Do not drive a car or operate machinery until you know how this medication affects you.
Do not take this medication if:
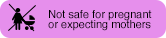
- you are pregnant women. Use in the treatment of cancer is justified only when the potential benefit outweighs the risk to the fetus.
- are breastfeeding
- if you abuse alcohol (alcoholism), have alcoholic liver disease, or have other chronic liver disease
- have immunodeficiency syndromes along with rheumatoid arthritis (RA) or psoriasis
- have preexisting blood dyscrasias, such as bone marrow hypoplasia, leukopenia, thrombocytopenia, or significant anemia along with RA or psoriasis
- have a known hypersensitivity to methotrexate
Methotrexate Food Interactions
Medicines can interact with certain foods. In some cases, this may be harmful and your doctor may advise you to avoid certain foods. In the case of methotrexate, there are no specific foods that you must exclude from your diet when receiving this medication.
Inform MD
Before taking methotrexate, tell your doctor about all of your medical conditions. Especially tell your doctor if you:
- are allergic to methotrexate or any of its ingredients
- have low blood folate levels
- have liver problems
- are pregnant or breastfeeding
- are having surgery, including dental surgery
Tell your doctor about all the medicines you take including prescription and non-prescription medicines, vitamins, and herbal supplements.
Methotrexate and Pregnancy
Tell your doctor if you are pregnant or plan to become pregnant.
The FDA categorizes medications based on safety for use during pregnancy. Five categories - A, B, C, D, and X, are used to classify the possible risks to an unborn baby when a medication is taken during pregnancy.
This medication falls into category X. Methotrexate may cause death or serious harm to your unborn baby.
Methotrexate and Lactation
Tell your doctor if you are breastfeeding or plan to breastfeed. You should not breastfeed while taking methotrexate as it is excreted into human breast milk and may harm your nursing baby.
Methotrexate Usage
Oral:
- Methotrexate comes as a tablet and solution to take by mouth. Your doctor will tell you how often you should take methotrexate. The schedule depends on the condition you have and on how your body responds to the medication.
- Depending on your condition, your dosing schedule may require you to take methotrexate once daily for several days, alternating with days when you do not take the medicine. Or, your dosing schedule may require you to take the medicine once a week. Your doctor may also start you on a low dose of the medicine and gradually increase your dose. Take methotrexate exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
- If you miss a dose, take it as soon as you remember. However, if it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule.
- Continue to take methotrexate even if you feel well. Do not stop taking methotrexate without talking to your doctor.
Injectable:
- Methotrexate injection comes as a powder to be mixed with liquid to be injected intramuscularly (into a muscle), intravenously (into a vein), intra-arterially (into an artery), or intrathecally (into the fluid-filled space of the spinal canal). The length of treatment depends on the types of drugs you are taking, how well your body responds to them, and the type of cancer or condition you have.
Methotrexate Dosage
Oral/Injectable
Take this medication exactly as prescribed by your doctor. Follow the directions on your prescription label carefully.
The dose your doctor recommends may be based on the following:
- the condition being treated
- other medical conditions you have
- other medications you are taking
- how you respond to this medication
- your weight
- your height
- your age
- your gender
Your doctor will adjust your dose based on lab values, how you respond and side effects you might experience.
- RA is 7.5 mg of an oral (by mouth) formulation once weekly or 2.5 mg at 12-hour intervals for 3 doses given as a course once weekly (oral)
- pJIA is 10 mg/m2 once weekly
- psoriasis is 10 to 25 mg once weekly by mouth or as an injection into the muscle, just under the skin, or into the vein or 2.5 mg at 12-hour intervals for three doses (oral only)
- choriocarcinoma and similar trophoblastic diseases (oral or IM formulation) is 15 mg to 30 mg by mouth daily for a 5-day course. Such courses are usually repeated for 3 to 5 times as required.
Head and neck cancer: The recommended dose is 40mg/m2 into the vein once a week.
Breast cancer: The recommended dose is 40mg/m2 into the vein once a week.
For leukemia:
- Maintenance therapy is 20 mg/m2 on a weekly basis.
For lymphoma:
<65 years old: the recommended dose is 300 mg/m2 once which is followed by 2,700 mg/m2 over the next 23 hours.
>65 years old: the recommended dose is 100 mg/m2 once which is followed by 900 mg/m2 over the next 23 hours.
For mycosis fungoides (cutaneous T cell lymphoma):
- The recommended dose is 5 mg to 50 mg once weekly. Methotrexate has also been administered twice weekly in doses ranging from 15 mg to 37.5 mg in those who have responded poorly to weekly therapy.
Methotrexate Overdose
If you take too much this medication, call your healthcare provider or local Poison Control Center, or seek emergency medical attention right away.
If this medication is administered by a healthcare provider in a medical setting, it is unlikely that an overdose will occur. However, if overdose is suspected, seek emergency medical attention.
Other Requirements
Oral:
- Store methotrexate tablets at room temperature.
- Store methotrexate oral solution at room temperature or in the refrigerator. If kept at room temperature, the oral solution should be discarded after 60 days.
- Protect from light.
- Keep this and all medications out of reach of children.
Injectable:
- Store at room temperatures; excursions permitted to 15° to 30°C (59° to 86°F).
- Protect from light.
- Retain in carton until time of use. Discard unused portion.
- This container closure is not made with natural rubber latex.
Methotrexate FDA Warning
WARNING:
-
METHOTREXATE SHOULD BE USED ONLY BY PHYSICIANS WHOSE KNOWLEDGE AND EXPERIENCE INCLUDE THE USE OF ANTIMETABOLITE THERAPY. BECAUSE OF THE POSSIBILITY OF SERIOUS TOXIC REACTIONS (WHICH CAN BE FATAL):
-
METHOTREXATE SHOULD BE USED ONLY IN LIFE THREATENING NEOPLASTIC DISEASES, OR IN PATIENTS WITH PSORIASIS OR RHEUMATOID ARTHRITIS WITH SEVERE, RECALCITRANT, DISABLING DISEASE WHICH IS NOT ADEQUATELY RESPONSIVE TO OTHER FORMS OF THERAPY.
-
DEATHS HAVE BEEN REPORTED WITH THE USE OF METHOTREXATE IN THE TREATMENT OF MALIGNANCY, PSORIASIS, AND RHEUMATOID ARTHRITIS. PATIENTS SHOULD BE CLOSELY MONITORED FOR BONE MARROW, LIVER, LUNG AND KIDNEY TOXICITIES.
-
PATIENTS SHOULD BE INFORMED BY THEIR PHYSICIAN OF THE RISKS INVOLVED AND BE UNDER A PHYSICIAN’S CARE THROUGHOUT THERAPY.
-
THE USE OF METHOTREXATE HIGH DOSE REGIMENS RECOMMENDED FOR OSTEOSARCOMA REQUIRES METICULOUS CARE. HIGH DOSE REGIMENS FOR OTHER NEOPLASTIC DISEASES ARE INVESTIGATIONAL AND A THERAPEUTIC ADVANTAGE HAS NOT BEEN ESTABLISHED. METHOTREXATE FORMULATIONS AND DILUENTS CONTAINING PRESERVATIVES MUST NOT BE USED FOR INTRATHECAL OR HIGH DOSE METHOTREXATE THERAPY
-
Methotrexate has been reported to cause fetal death and/or congenital anomalies.Therefore, it is not recommended for women of childbearing potential unless there is clear medical evidence that the benefits can be expected to outweigh the considered risks. Pregnant women with psoriasis or rheumatoid arthritis should not receive methotrexate.
-
Methotrexate elimination is reduced in patients with impaired renal functions, ascites, or pleural effusions. Such patients require especially careful monitoring for toxicity, and require dose reduction or, in some cases, discontinuation of methotrexate administration
-
Unexpectedly severe (sometimes fatal) bone marrow suppression, aplastic anemia, and gastrointestinal toxicity have been reported with concomitant administration of methotrexate (usually in high dosage) along with some nonsteroidal anti-inflammatory drugs (NSAIDs).
-
Methotrexate causes hepatotoxicity, fibrosis and cirrhosis, but generally only after prolonged use. Acutely, liver enzyme elevations are frequently seen. These are usually transient and asymptomatic, and also do not appear predictive of subsequent hepatic disease. Liver biopsy after sustained use often shows histologic changes, and fibrosis and cirrhosis have been reported; these latter lesions may not be preceded by symptoms or abnormal liver function tests in the psoriasis population. For this reason, periodic liver biopsies are usually recommended for psoriatic patients who are under long-term treatment. Persistent abnormalities in liver function tests may precede appearance of fibrosis or cirrhosis in the rheumatoid arthritis population.
-
Methotrexate-induced lung disease, including acute or chronic interstitial pneumonitis, is a potentially dangerous lesion, which may occur acutely at any time during therapy and has been reported at low doses. It is not always fully reversible and fatalities have been reported. Pulmonary symptoms (especially a dry, nonproductive cough) may require interruption of treatment and careful investigation.
-
Diarrhea and ulcerative stomatitis require interruption of therapy: otherwise, hemorrhagic enteritis and death from intestinal perforation may occur. Malignant lymphomas, which may regress following withdrawal of methotrexate, may occur in patients receiving low-dose methotrexate and, thus, may not require cytotoxic treatment. Discontinue methotrexate first and, if the lymphoma does not regress, appropriate treatment should be instituted.
-
Like other cytotoxic drugs, methotrexate may induce“tumor lysis syndrome” in patients with rapidly growing tumors. Appropriate supportive and pharmacologic measures may prevent or alleviate this complication.
-
Severe, occasionally fatal, skin reactions have been reported following single or multiple doses of methotrexate. Reactions have occurred within days of oral, intramuscular, intravenous, or intrathecal methotrexate administration. Recovery has been reported with discontinuation of therapy.
-
Potentially fatal opportunistic infections, especially Pneumocystis carinii pneumonia, may occur with methotrexate therapy.
-
Methotrexate given concomitantly with radiotherapy may increase the risk of soft tissue necrosis and osteonecrosis.
