Depakene
Depakene is used to treat certain types of seizures. It can be used alone or with other medications.



Depakene Overview
Depakene is a prescription medication used to treat seizures and manic episodes in people with bipolar disorder and to prevent migraines. Depakene belongs to a group of drugs called anticonvulsants or anti-epileptic drugs. These work by increasing the amount of certain chemicals in the brain.
This medication comes in capsule and syrup forms. It is usually taken at least 2 times a day.
Common side effects of Depakene include upset stomach, constipation or diarrhea, nausea, and headache.
Depakene can cause drowsiness, dizziness, or blurred vision. Do not drive or operate heavy machinery until you know how Depakene affects you.
How was your experience with ?
Depakene Cautionary Labels
Uses of Depakene
Depakene is a prescription medication used to treat seizures.
This medication may be prescribed for other uses. Ask your doctor or pharmacist for more information.
Generic
Divalproex Sodium
For more information on this medication choose from the list of selections below.
Depakene Drug Class
Depakene is part of the drug class:
Side Effects of Depakene
Serious side effects have been reported with Depakene. See “Depakene Precautions” section.
Common side effects of Depakene include:
- upset stomach and nausea
- blurred vision
- constipation
- depression
- diarrhea
- dizziness
- drowsiness
- headache, increased appetite
- insomnia
- nervousness
- rash
- tremor
- vomiting
- weight gain or weight loss
- changes in appetite
- back pain
- changes in mood or mood swings
- abnormal thinking
- ringing in the ears
- hair loss
This is not a complete list of Depakene side effects. Ask your doctor or pharmacist for more information.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Depakene Interactions
Tell your doctor about all the medicines you take including prescription and non-prescription medicines, vitamins, and herbal supplements. Especially tell your doctor if you take:
- acyclovir (Zovirax)
- aspirin
- antibiotics such as meropenem (Merrem), imipenem (Primaxin), doripenem (Doribax), and ertapenem (Invanz)
- anticoagulants such as warfarin (Coumadin, Jantoven)
- clonazepam (Klonopin)
- medications for anxiety or mental illness
- other medications for seizures such as carbamazepine (Tegretol), ethosuximide (Zarontin), felbamate (Felbatol), lamotrigine (Lamictal), mephobarbital (Mebaral), phenobarbital, phenytoin (Dilantin), primidone (Mysoline), and topiramate (Topamax)
- rifampin (Rifadin)
- sedatives, tranquilizers, or sleeping pills such as diazepam (Valium)
- tricyclic antidepressants such as amitryptyline (Elavil) and nortryptyline (Pamelor, Aventyl)
- tolbutamide
- zidovudine (Retovir, Trizivir)
This is not a complete list of Depakene drug interactions. Ask your doctor or pharmacist for more information.
Depakene Precautions
Serious side effects have been reported with Depakene including:
- Liver toxicity: Your doctor will want to monitor your liver function tests. Tell your healthcare provider right away if you have some or all of the following symptoms of liver toxicity:
- yellowish tint to eyes and skih
- stomach pain and swelling
- itchiness
- dark urine color and/or pale stool color
- bloody or tar-colored stool
- fatigue
- nausea and/or loss of appetite
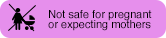
- Depakene may harm your unborn baby.
- If you take Depakene during pregnancy for any medical condition, your baby is at risk for serious birth defects. The most common birth defects with divalproex affect the brain and spinal cord and are called spina bifida or neural tube defects. These defects occur in 1 to 2 out of every 100 babies born to mothers who use this medicine during pregnancy. These defects can begin in the first month, even before you know you are pregnant. Other birth defects can happen.
- Birth defects may occur even in children born to women who are not taking any medicines and do not have other risk factors.
- Taking folic acid supplements before getting pregnant and during early pregnancy can lower the chance of having a baby with a neural tube defect.
- If you take Depakene during pregnancy for any medical condition, your child is at risk for having a lower IQ.
- There may be other medicines to treat your condition that have a lower chance of causing birth defects and decreased IQ in your child.
- Women who are pregnant must not take Depakene to prevent migraine headaches.
- All women of childbearing age should talk to their healthcare provider about using other possible treatments instead of Depakene. If the decision is made to use divalproex, you should use effective birth control (contraception).
- Tell your healthcare provider right away if you become pregnant while taking Depakene . You and your healthcare provider should decide if you will continue to take divalproex while you are pregnant.
- Pregnancy Registry: If you become pregnant while taking divalproex, talk to your healthcare provider about registering with the North American Antiepileptic Drug Pregnancy Registry. You can enroll in this registry by calling 1888-233-2334. The purpose of this registry is to collect information about the safety of antiepileptic drugs during pregnancy.
- Pancreatitis: Tell your healthcare provider right away if you have some or all of the following symptoms of pancreatitis:
- a swollen and tender abdomen
- nausea
- vomiting
- fever
- a fast pulse
- Suicidal behavior or ideation: Tell your healthcare provider right away if you have some or all of the following symptoms of suicidal thoughts or actions:
- new or worsening feelings of depression
- suicidal thoughts or behavior
- any unusual changes in mood or behavior
- Thrombocytopenia (low platelet counts): Your doctor may want monitor platelet counts and bleeding tests. Tell your healthcare provider right away if you have some or all of the following symptoms thrombocytopenia:
- bleeding that does not stop
- bruising
- Hyperammonemia and hyperammonemic encephalopathy (a condition of brain dysfunction): Tell your healthcare provider right away if you have some or all of the following symptoms of encephalopathy:
- inexplicable tiredness and fatigue
- vomiting
- changes in mental status
- Hypothermia: A drop in body temperature to 95 degrees Fahrenheit or less (hypothermia) has been reported with Depakote therapy.Tell your healthcare provider right away if you have some or all of the following symptoms of hypothermia:
- fatigue
- confusion
- coma
- changes heart rate, blood pressure, or breathing
- Multi-organ hypersensitivity (allergic) reaction: Tell your healthcare provider right away if you have some or all of the following symptoms of an allergic reaction:
- fever
- rash
- decreased urination
- joint pain
- weakness or loss of energy
- Because this reaction may have effects on many organs of the body, not all symptoms are included.
- Somnolence (drowsiness): This effect is seen especially in the elderly population. The dosage of divalproex should be increased slowly and with regular monitoring for fluid and nutritional intake.
Depakene can cause drowsiness, dizziness, and blurred vision. Do not drive or operate heavy machinery until you know how Depakene affects you.
Do not take Depaken if you:
- are allergic to Depakene or to any of its ingredients
- have liver disease or significant liver dysfunction
- have a known mitochondrial disorder or suspect a mitochondrial disorder in children younger than 2 years old
- have urea cycle disorders
Depakene Food Interactions
Medicines can interact with certain foods. In some cases, this may be harmful and your doctor may advise you to avoid certain foods. In the case of Depakene, there are no specific foods that you must exclude from your diet when receiving Depakote.
Inform MD
Before taking Depakene, tell your doctor about all of your medical conditions. Especially tell your doctor if you:
- drink alcohol
- have or have had depression, mood problems, or suicidal thoughts or behavior
- have episodes of confusion, especially during pregnancy or childbirth
- have difficulty coordinating movements
- have human immunodeficiency virus (HIV) or cytomegalovirus (CMV)
- have urea cycle disorders
- have liver or kidney problems
- are pregnant or breastfeeding
Tell your doctor about all the medicines you take including prescription and non-prescription medicines, vitamins, and herbal supplements.
Depakene and Pregnancy
Tell your doctor if you are pregnant or plan to become pregnant. Depakene may harm your unborn baby.
The FDA categorizes medications based on safety for use during pregnancy. Five categories - A, B, C, D, and X, are used to classify the possible risks to an unborn baby when a medication is taken during pregnancy.
Depakene falls into category D. There is evidence of risk to the unborn baby based on studies in humans or adverse reaction data, but this medication may be given to a pregnant woman if her healthcare provider believes that its benefits to the pregnant woman outweigh any possible risks to her unborn baby.
Depakene and Lactation
Tell your doctor if you are breastfeeding or plan to breastfeed.
Depakene is excreted in human milk. Caution should be exercised when Depakene is given to a nursing mother.
Depakene Usage
Take Depakene exactly as prescribed.
This medication comes in capsule and syrup forms. It is usually taken at least 2 times a day.
The syrup should not be mixed with carbonated beverages.
If you miss a dose, take the missed dose as soon as you remember. If it is almost time for the next dose, skip the missed dose and take your next dose at the regular time. Do not take two doses of Depakene at the same time.
Depakene Dosage
Take divalproex exactly as prescribed by your doctor. Follow the directions on your prescription label carefully. The dosage will vary, depending on the indication and response.
The dose your doctor recommends may be based on the following:
- the condition being treated
- other medical conditions you have
- other medications you are taking
- how you respond to this medication
- your weight
- your age
The recommended starting of divalproex for the treatment of complex partial seizures is 10 to 15 mg/kg/day. The dose is increased at 1-week intervals by 5 to 10 mg/kg/day to achieve clinical response. The maximum recommended dosage is 60 mg/kg/day.
The recommended starting dose of divalproex for the treatment of absence seizures is 15 mg/kg/day. The dose is increased at 1-week intervals by 5 to 10 mg/kg/day until seizure control is achieved or side effects are not tolerable. The maximum recommended dosage is 60 mg/kg/day.
Depakene Overdose
If you take too much Depakene, call your healthcare provider or local Poison Control Center, or seek emergency medical attention right away.
If Depakene is administed by a healthcare provider in a medical setting, it is unlikely that an overdose will occur. However, if overdose is suspected, seek emergency medical attention.
Other Requirements
Store Depakene at room temperature.
Keep this and all medicines out of the reach of children.
Depakene FDA Warning
Hepatotoxicity
Hepatic failure resulting in fatalities has occurred in patients receiving valproate and its derivatives. Children under the age of two years are at a considerably increased risk of developing fatal hepatotoxicity, especially those on multiple anticonvulsants, those with congenital metabolic disorders, those with severe seizure disorders accompanied by mental retardation, and those with organic brain disease. When Depakene is used in this patient group, it should be used with extreme caution and as a sole agent. The benefits of therapy should be weighed against the risks. The incidence of fatal hepatotoxicity decreases considerably in progressively older patient groups.
These incidents usually have occurred during the first six months of treatment. Serious or fatal hepatotoxicity may be preceded by non-specific symptoms such as malaise, weakness, lethargy, facial edema, anorexia, and vomiting. In patients with epilepsy, a loss of seizure control may also occur. Patients should be monitored closely for appearance of these symptoms. Liver function tests should be performed prior to therapy and at frequent intervals thereafter, especially during the first six months.
Fetal Risk
Pancreatitis
Cases of life-threatening pancreatitis have been reported in both children and adults receiving valproate. Some of the cases have been described as hemorrhagic with a rapid progression from initial symptoms to death. Cases have been reported shortly after initial use as well as after several years of use. Patients and guardians should be warned that abdominal pain, nausea, vomiting, and/or anorexia can be symptoms of pancreatitis that require prompt medical evaluation. If pancreatitis is diagnosed, valproate should ordinarily be discontinued. Alternative treatment for the underlying medical condition should be initiated as clinically indicated.

